GLAUCOMA
Glaucoma is a disease that results in progressive loss in your peripheral or side vision, and can eventually cause blindness. In glaucoma, damage occurs to your eye’s optic nerve, the neural “signal cable” that allows the visual information from the eye to be transmitted to the brain so that you can see. Increased awareness about this condition is important because with early detection and treatment, the eye sight can often be protected.
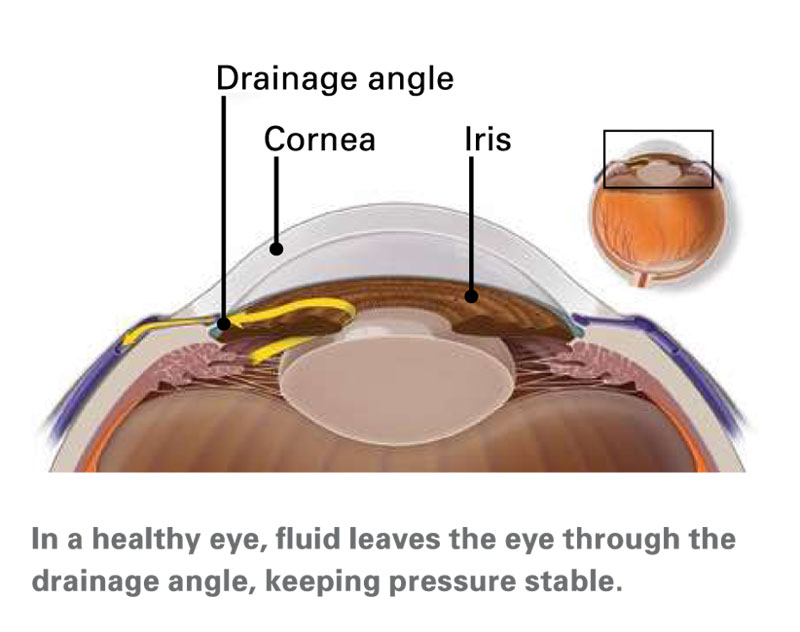
Image from American Academy of Ophthalmology: Glaucoma
What causes glaucoma?
The most common cause of glaucoma is higher pressure inside the eye (the intraocular pressure or IOP), which then causes stress on the optic nerve and thus progressive loss of its nerve fibres. The eye can be thought of like a balloon, filled up with fluid called the aqueous humor, which is in a constant state of secretion into the eye and its equally balanced drainage out from the eye when in good health. However, if this balanced state is disturbed because the drainage pathway is not working properly (like clogged up kitchen sink drain), the fluid inside the eye and eye pressure builds up, resulting in disease. Similar to high blood pressure being not good for your cardiovascular health, having high eye pressure is unhealthy for your eye. In addition to this, there is also a form of glaucoma called “normal tension” glaucoma where the eye pressure is not necessarily that high, but the optic nerve is still susceptible to glaucomatous damage. The main treatable factor in glaucoma is to lower the eye pressure.
Who is at risk for glaucoma?
Some people have a higher than average risk of glaucoma. The known risk factors include:
- Age over 40 years
- Have family members with glaucoma (genetic)
- Asian, African or Hispanic heritage
- High eye pressure
- Being long- or short-sighted (needing strong prescription glasses)
- Previous eye injury or trauma
- Use of long-term steroid medications
- Migraine sufferer
- Other eye conditions such as uveitis, cataract, diabetic retinopathy
Types of glaucoma
There are two major types of glaucoma:
1. Chronic open-angle glaucoma
This is the most common type of glaucoma. Chronic glaucoma happens gradually and so in most cases, there are no symptoms. This type of glaucoma is painless and causes no noticeable vision changes until it is much more advanced. This highlights the importance of regular eye examination in those at potential risk of developing glaucoma, even if there are no perceived problems with vision or eye discomfort. Some people can also have a type of glaucoma called “normal tension glaucoma”, where the eye pressure is not high but their optic nerves are susceptible to even what we consider to be “within normal range” eye pressure. Often, such patients with glaucoma also have wider fluctuations in their eye pressures from different times of the day or from day to day.
2. Angle-closure glaucoma (also called, “acute narrow-angle glaucoma”)
Angle-closure glaucoma is less common and happens when someone’s iris (the coloured part of the eye) is very close to the drainage angle in their eye. “Angle closure” occurs when this angle inside the eye gets progressively more narrowed and finally the iris ends up blocking the drainage angle and the eye pressure rises very quickly. In this type of “acute glaucoma”, there is very high eye pressure that causes symptoms such as eye pain, headache and blurred vision. This is an eye emergency that can lead to blindness and so you need to seek urgent eye specialist treatment.
In the chronic form of angle-closure glaucoma, a similar problem with narrow angles results in a very slow and gradual closure of the drainage angle. Because this process can be very slow, this results in a gradual rise in the eye pressure and so there is often no symptoms in early stages of the disease. Treatments for angle-closure glaucoma are often aimed at trying to open up this narrowed anterior chamber angle with laser, medications or eye surgery.
How is glaucoma diagnosed?
Glaucoma can only be diagnosed by your optometrist or eye doctor after a complete eye examination including relevant investigation tests such as visual field and OCT scan. For persons with risk factor(s) for developing glaucoma, such examinations on a regular and periodic basis is vital, because there is no symptoms at all for most forms of glaucoma. Early diagnosis is important because appropriate treatment can prevent vision loss from glaucoma. In contrast, there is no way to recover lost vision from advanced glaucoma damage that has been detected too late.
Some of the tests performed in a glaucoma examination by your eye specialist include:
- Measure your eye pressure
- Inspect your eye’s drainage angle to see if it is narrow (gonioscopy & anterior segment OCT scan)
- Examine your optic nerve for signs of glaucoma damage
- Measure the thickness of your cornea (the front window of the eye)
- Test your peripheral (side) vision (visual field examination)
- Take photos and scans of your optic nerve (including OCT scan)
How is glaucoma treated?
The main way of treating glaucoma is to lower the eye (intraocular) pressure. There is no magic number for an acceptable intraocular pressure but the aim is to lower the eye pressure to a safe level for your eye, so that further damage to the optic nerve is prevented. One or more of the following treatments may be used by your ophthalmologist to treat your glaucoma.
Glaucoma eye drop medicine
This is the most common form of treatment for glaucoma. There are various eye drop medicines available (eg. Xalatan, Timolol, Alphagan, Ganfort PF). They work in slightly different ways but their shared goal is to lower the eye pressure, by either reducing the amount of fluid secreted into the eye or increasing its drainage outflow from the eye. Often, glaucoma eye drops need to be used every day as there is currently no cure for glaucoma. Depending on the severity of your glaucoma, a combination of the eye drops may be used to achieve even lower eye pressure. All medications, including eye drops, can have side effects. Your doctor will explain these potential side effects to look out for and monitor your response to treatment. Some of the side effects from glaucoma eye drops include red or itchy eyes, but be aware that some are remote from the eye such as shortness of breath.Laser treatment
There are two main types of laser treatment for glaucoma. These treatments are very safe, painless and can be done in the clinic by your eye doctor (does not need hospital admission). Such laser treatment may be offered as a standalone treatment or as combination treatment with medical eye drop therapy.1. Trabeculoplasty or SLT laser
This treatment is for people who have open-angle glaucoma. The laser helps to make the drainage angle work better and hence lowers the eye pressure. This is particularly useful for persons who have multiple allergies to glaucoma eye drops or those who are not good at remembering to use the eye drops every day.
Watch Dr Chang explaining Selective Laser Trabeculoplasty (SLT) in this video >>2. Laser iridotomy
This treatment is for people who have angle-closure glaucoma. The laser treatment creates a tiny hole in the iris to help widen the narrowed angle and thereby improve fluid outflow via the drainage angle. Laser iridotomy can also be performed as a preventative treatment for particularly predisposed persons, so that they are protected from developing glaucoma later.Minimally Invasive Glaucoma Surgery (MIGS)
(such as microtrabecular glaucoma stent implants)
This is a recent advancement in the surgical treatment option for glaucoma that has proven efficacy and safety profile. In fact, MIGS has been shown to be safer than the more traditional glaucoma surgeries and are particularly useful for patients with mild to moderate severity glaucoma. Micro-trabecular glaucoma stents (such as Glaukos iStent inject) are implanted into the drainage angle, allowing improved outflow of the fluid from inside the eye, with resultant lowering of the eye pressure. Another additional advantage of such MIGS surgery is that they can be safely performed at the same time as your cataract surgery, without the need for a separate procedure. Dr John Chang can assess and explain whether you would be suitable for this type of combined cataract and glaucoma micro-stent implant operation.
Watch Dr Chang explaining Minimally Invasive Glaucoma Surgery (MIGS) in this video >>Glaucoma surgery
(such as trabeculectomy or glaucoma drainage tube devices)
Traditional glaucoma surgery involves creating a new drainage channel for the aqueous humor to leave the eye. This type of surgery is often the most effective way of achieving a very low eye pressure, which is needed for more severe glaucoma. As effective as they are, such surgery also has relatively higher chances of problems arising from the procedure and so these are generally reserved for glaucoma that cannot be stabilized despite the above medical and laser treatments have been tried first. Fortunately, traditional glaucoma surgery are being required less commonly now due to the advances in better medical, laser and microinvasive glaucoma surgery options.
If you would like to find out what glaucoma treatments are suitable for you, please call Eastwood Eye Specialists for an appointment.