Diabetic Retinopathy
Eye disease called diabetic retinopathy can develop in people with diabetes (either type 1 or 2) and this is one of the leading causes of treatable vision loss in diabetics. This occurs when high blood sugar levels (over many years) causes damage to the blood vessels in the retina.
The damaged blood vessels can block up or leak causing bleeding and impaired blood circulation, resulting in damage to the retina or the “film in the camera” of the eye, which is vitally important for vision. Damaged retina can lead to irreversible vision loss and blindness.
Stages of diabetic retinopathy
There are two main stages of diabetic retinopathy.
1. Non-proliferative diabetic retinopathy (NPDR)
Non-proliferative retinopathy is the early stage of diabetic eye disease and many people with diabetes have it, often without any symptoms. With NPDR, the damaged blood vessels in the retina leak, resulting in swelling and bleeding of the retina. When the central part of the retina, called the macula gets swollen, it is called “macular oedema”. Macular oedema is the most common reason why people with diabetes lose their vision.
2. Proliferative diabetic retinopathy (PDR)
Proliferative retinopathy is a more advanced stage of diabetic retinopathy and it is less common. PDR is characterized by more severe impairment of the retinal circulation due to blockage of the damaged retinal blood vessels. When this happens, the retina undergoes distress due to the consequent lack of vital nutrients and oxygen being supplied, and it starts growing abnormal new blood vessels in response. Such abnormal blood vessels are fragile and bleed easily and can lead to development of fibrous scar tissues that pull off the retina (resulting in retinal detachment). Both of these complications can lead to blindness.
What are the symptoms of diabetic retinopathy?
Most often, diabetic retinopathy causes no symptoms (such as eye pain or difficulty seeing) in its early stages and hence affected persons may not even know that they have this sight-threatening condition. This is why it is critically important that all persons with diabetes should have regular periodic screening eye examinations with their eye specialist. Regardless of whether there are any difficulty with vision, all diabetic persons must have their eyes and retina examined so that early diabetic retinopathy is detected and vision loss prevented. Eventually, as diabetic retinopathy gets worse, it will start causing noticeable problems including blurry vision, difficulty reading, abrupt onset of numerous floaters, or even sudden onset of severe vision loss.
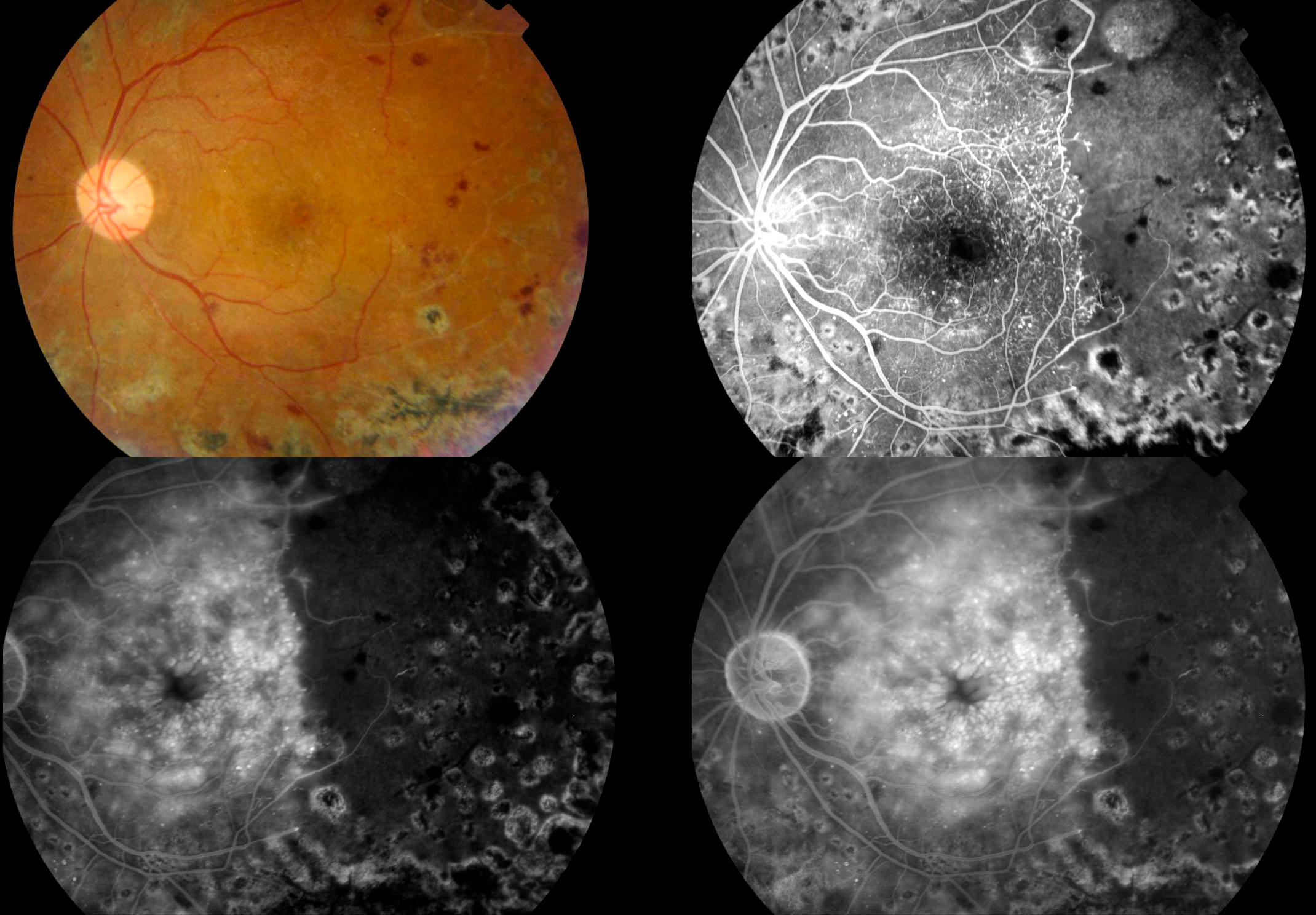
Retinal imaging in a patient with diabetic retinopathy. The first colour photo shows the appearance of the retina as seen by the eye specialist using specialised equipment. Red blotches are bleeds into the retina. The sequence of black and white pictures is retinal angiography, which shows leakage from the damaged retinal blood vessels (white, bright areas) and to the right of this, the darker area represents areas of the retina where there is insufficient blood flow due to the blockage of blood vessels from severe diabetic retinopathy.
Who is at risk of diabetic retinopathy?
Anyone who has diabetes is at risk of developing diabetic eye disease. In particular, the following groups are at higher risk and should be even more careful in ensuring that their eyes are regularly examined:
- Longer duration of diabetes
- Poor blood sugar (high BSL) control
- High blood pressure & high cholesterol
- Cigarette smoking
- Other diabetic complications such as poor kidney function, diabetic foot ulcers, peripheral neuropathy
- Pregnancy
Dr John Chang has been part of an Australian research team that have discovered new genes that places certain people at higher risk of developing diabetic retinopathy and in particular for certain vision-threatening problems due to their diabetic retinopathy. Details of his cutting edge clinical research in this field can be found under the publication list under his biography section.
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed by your eye specialist looking through a special microscope and optical lenses to see the inside of your eye (retinal examination). To perform a detailed comprehensive retinal examination, dilating eye drops to widen your pupils is necessary.
Specialised retinal imaging tests may also be required depending on the findings, and these include Optical Coherence Tomography (OCT) scans. These use laser light and are quick, comfortable and safe examinations that can be done in the eye specialist clinic during the same visit. OCT scans of the macula may detect early swelling. OCT angiography (OCT-A) allows a high-resolution imaging of the retinal blood vessels without the need for traditional dye injection into a vein. In summary, eye examinations to diagnose and monitor diabetic retinopathy can be done comfortably, relatively quickly and non-invasively at a clinic visit, without need to go to hospital.
How is diabetic retinopathy treated?
Treatment of diabetic retinopathy depends on the type and severity of your eye condition as well as whether there are vision threatening problems such as swelling of the macula or abnormal blood vessels that are bleeding. When diabetic retinopathy is mild and vision is unaffected, your eye specialist may not recommend any eye treatment but keep you under ongoing monitoring. Dr Chang will tailor the treatment options for your specific circumstances. Most patients only need eye check up only once or twice a year.
Broadly speaking, treatment options include:
- Medical control of your blood sugar level (BSL), blood pressure and cholesterol.
- “Anti-VEGF” eye medications (such as Lucentis, Avastin, Eylea and Vabysmo): These help to reduce the swelling of the macula, preventing vision loss and even improving vision in some cases. This treatment is given by injections into the eye. This is a very safe and effective treatment that is given in the procedure room of the clinic.
- Retinal laser treatment: Non-invasive laser therapy may be used to help seal off leaking blood vessels. This can reduce swelling of the retina and may avoid or delay the need for eye injection treatment. Sometimes retinal laser may be used in combination with eye injection therapy. Laser treatment can also help shrink abnormal blood vessels in more advanced diabetic retinopathy and prevent them from growing back again. Such laser treatment can be comfortably done in the clinic.
- Steroid medicine: Ozurdex is a slow-release steroid implant that can be injected into the eye to treat macula swelling from diabetic retinopathy. One of the key advantages of this treatment is that the slow-release delivery of this medicine means that there is a longer lasting therapeutic benefit and hence less frequent treatments being required.
- Retinal surgery such as retinal detachment operation or vitrectomy may be required for more advanced diabetic retinopathy. Proliferative retinopathy can cause vision loss from large bleed inside the eye or retinal detachment from scar tissues, and such severe cases may require surgery in addition to other treatments. Vitreoretinal surgery removes the vitreous gel and blood from inside the eye, as well as removes scar tissues from the retina and re-attach it. With early diagnosis and appropriate treatment, such advanced diabetic eye disease and the need for surgery can be avoided.
Preventing vision loss from diabetic retinopathy
Diabetic retinopathy is one of the leading causes of vision loss and blindness in Australia. It can be particularly devasting when this afflicts younger persons, and can impair their ability to drive, work or study. However, with appropriate treatment, vision loss can be prevented.
- All persons with diabetes (type 1 or 2) must have their eyes examined regularly (at least once a year). Diabetic retinopathy may be found even before you notice any problems with your vision.
- Ensure that you have good control of your blood sugar level (BSL), blood pressure, and cholesterol. This is managed by your GP and diabetes specialist (endocrinologist).
- If you notice any change in the vision in one or both eyes, contact your eye specialist without delay.
- Get treatment for diabetic retinopathy as soon as possible. Early treatment before it becomes more severe is the best way to prevent vision loss.
If you have been diagnosed with diabetes, it is important to have your eyes regularly monitored by an eye specialist. Please call Eastwood Eye Specialists for an appointment.